Abstract
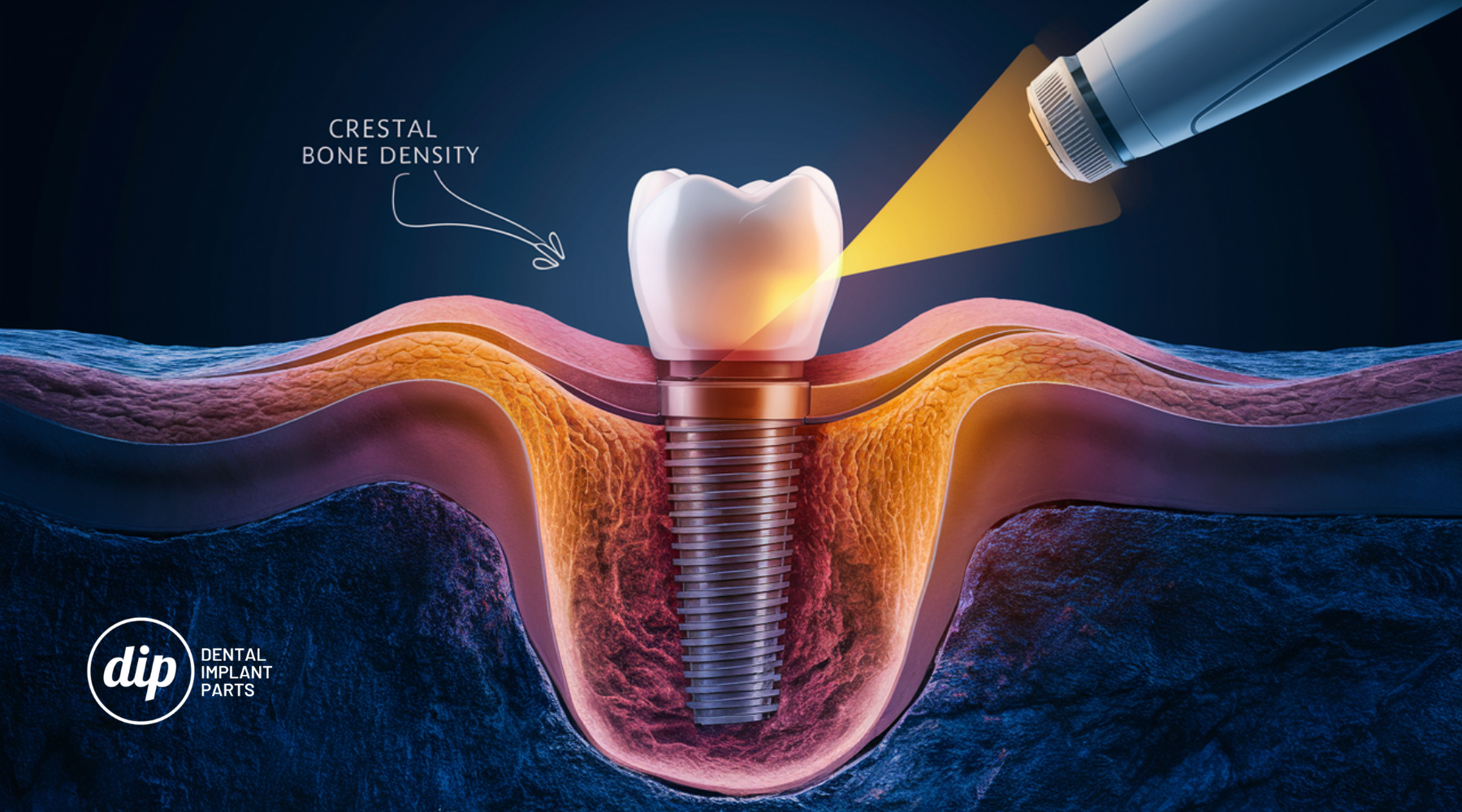
Dental implants have become an essential part of modern dentistry. The initial bone resorption at the implant surface significantly impacts implant success. Bone alterations around the implant are a critical factor in determining the implant's effectiveness. Reducing peri-implant crestal bone loss has always been a primary goal. Various procedures in dental implantology aim to enhance implant stability and bone healing. Photobiomodulation techniques, also known as low-level laser therapy (LLLT), have gained popularity for their ability to accelerate osseointegration by inducing cellular metabolism and stimulating tissue healing. This case study details implant loading in a patient treated with photobiomodulation to achieve implant stability in compromised bone type or D4.
Introduction
Patients with dental anomalies are increasingly turning to dental implants for their excellent aesthetics, high success rates, and functional benefits. However, the risk of implant failure due to insufficient osseointegration remains a concern for many patients. Several factors influence the osseointegration process, including physical, chemical, and biological elements. One such biological element is photobiomodulation therapy (PBMT), also known as low-intensity laser therapy. For over three decades, LLLT has been used in the medical field without reported side effects. It involves red beam or near-infrared laser therapies with low energy density and output power that do not raise normal body or tissue temperature, offering non-thermal and biostimulative properties. By inducing cytokines and growth factors that promote fibroblast migration and proliferation, LLLT accelerates angiogenesis, enhances mesenchymal cell differentiation into osteoblasts, and improves osteoblast adhesion to the surface of titanium implants, all contributing to bone regeneration. Additionally, studies show that LLLT increases the creation of bone nodules and improves the mechanical strength of the implant-bone interface. This case report describes implant loading in a patient with D4 or compromised bone type, treated using photobiomodulation to achieve implant stability and prosthetic rehabilitation.
Case Presentation
Patient Information A 45-year-old male patient presented with a complaint of missing teeth in the lower left back region for the past two years, seeking a fixed replacement. The patient had a medical history of diabetes and was currently under medication.
Clinical Findings Oral examination revealed missing teeth #35 and #36, with the edentulous ridge appearing resorbed.
Investigations Cone beam computed tomography (CBCT) measured the bone density at 320 HU, categorizing the bone as D4 type or compromised bone.
Treatment Plan Diagnostic impressions were made using irreversible hydrocolloid impression material. Various treatment options were discussed, including tooth-supported fixed dental prosthesis, conventional implants with bone augmentation, and conventional implants with photobiomodulation therapy. With the patient's consent, conventional implants with photobiomodulation therapy were chosen.
Using a standard surgical technique, the mandibular posterior edentulous site was implanted. Asepsis was maintained throughout the procedure. Local anesthesia was administered, and a full-thickness mucoperiosteal flap was lifted. Osteotomy was performed with saline irrigation, and an implant fixture (3.8 mm diameter, 11 mm length) was inserted, achieving good primary stability (20 Ncm torque).
Photobiomodulation therapy was administered before suturing using a diode laser (epic10, BIOLASE, Inc.). Protective eyewear was worn by both patient and clinician. The laser specifications were a diode laser operating at 940 nm wavelength, 100 mW output power, 0.2826 cm² spot area, and 354.6 mW/cm² power density. Laser radiation was applied for 40 seconds on the buccal and palatal sides of the implant site. The total energy used was 8 J per session.
Follow-up laser treatments were conducted on days 2, 4, 6, 8, 10, and 12, with a total dose of 56 J. Post-surgery, the patient was prescribed antibiotics, pain relievers, and chlorhexidine mouthwash. A CBCT taken after three months showed improved bone density (800 HU).
Prosthetic Phase Metal-ceramic crowns were fabricated for the patient after the second stage of surgery.
Follow-Up and Outcome The patient was evaluated three months post-procedure, showing satisfactory prosthesis results.
Discussion
Photobiomodulation therapy was chosen for this patient due to its proven effects on compromised bone. LLLT uses light-emitting diodes or lasers applied to specific tissues, potentially altering biological processes. Research indicates that LLLT may impact osteoblasts by increasing mitochondrial activity, ATP synthesis, and reactive oxygen species production, leading to increased osteoblast proliferation and differentiation.
A study by Matys et al. suggests that fluence between 1 and 10 J/cm² achieves optimal biological reactions. In this case, 8 J/cm² was used to enhance secondary implant stability. CBCT analysis showed significant bone density improvement three months post-LLLT.
The literature indicates that near-infrared wavelengths (780-1100 nm) penetrate deeper tissues, with the Biolase laser (940 nm) chosen for this case falling within this range. The application of LLLT in dentistry, particularly oral implantology, has been extensively researched, showing benefits in enhancing primary stability during osseointegration.
Conclusion
Photobiomodulation with LLLT can improve crestal bone levels and accelerate osseointegration, enhancing implant success rates, especially in patients with compromised bone. By optimizing photobiomodulation procedures and understanding its advantages and limitations, practitioners can achieve better patient outcomes and satisfaction.
** Credit to cureus.com